Mental health policies, driven by advocacy and evidence-based practices, significantly improve access to quality care like Castle Rock Chronic Pain Therapy (CRCPT). Integrated healthcare systems and community programs enhance coordination and accessibility for diverse populations. CRCPT's success demonstrates a collaborative approach involving healthcare providers, policymakers, and advocates, leading to improved emotional healing and inner strength development for chronic pain sufferers. The program's multifaceted strategy includes policy analysis, risk management planning, and lobbying efforts resulting in expanded coverage and increased access to specialized treatments, setting a precedent for enhanced mental health service delivery.
Mental health policy analysis and advocacy are vital components in ensuring equitable access to quality care. This article delves into the intricate relationship between mental health policies and their profound impact on treatment accessibility. We explore the power of advocacy in shaping effective strategies, using Castle Rock Chronic Pain Therapy as a compelling case study demonstrating successful policy analysis and its ripple effects. By examining these aspects, we aim to highlight innovative approaches to improve mental healthcare systems.
- Understanding Mental Health Policy and Its Impact on Access to Care
- The Role of Advocacy in Shaping Effective Mental Health Policies
- Castle Rock Chronic Pain Therapy: A Case Study in Policy Analysis and Advocacy Success
Understanding Mental Health Policy and Its Impact on Access to Care

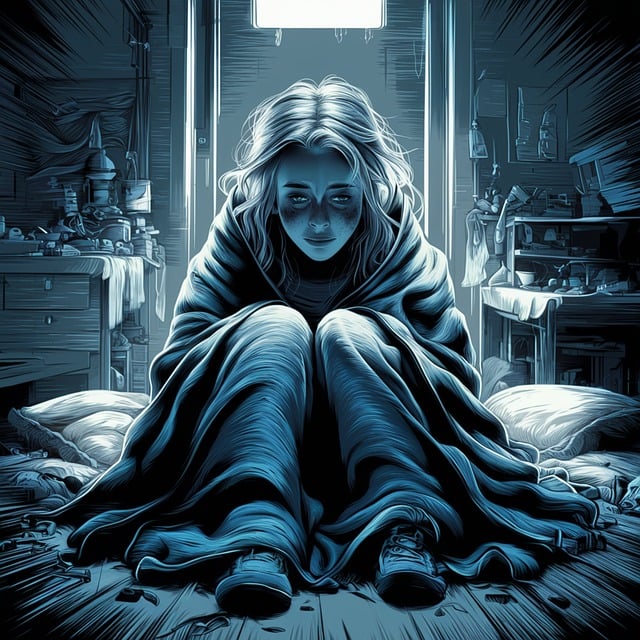
Mental health policy plays a pivotal role in shaping access to care for individuals grappling with various conditions, including Castle Rock Chronic Pain Therapy. Effective policies ensure that evidence-based treatments and support services are readily available, breaking down barriers to care. By implementing comprehensive legislation, governments can promote early intervention and prevent the escalation of mental health issues. This, in turn, fosters better outcomes and reduces the societal burden associated with untreated or inadequately treated conditions.
Understanding the intricate relationship between policy and access is crucial. For instance, policies that advocate for integrated healthcare systems can improve coordination among primary care providers and specialized therapists. Additionally, initiatives focusing on community-based programs, such as Stress Management Workshops Organization or Social Skills Training, enhance support networks, making care more accessible and acceptable to diverse populations. Such strategic interventions contribute to a more inclusive and responsive mental health ecosystem.
The Role of Advocacy in Shaping Effective Mental Health Policies

Advocacy plays a pivotal role in shaping effective mental health policies. It brings attention to critical issues within the field, ensuring that decisions are informed by real-world challenges faced by individuals seeking support for their mental well-being. Through advocacy, voices previously marginalized gain recognition, leading to more inclusive and responsive policies. This is particularly relevant when addressing complex conditions like Castle Rock Chronic Pain Therapy, where a holistic approach is necessary, encompassing not just medical treatment but also psychological and social interventions.
The power of advocacy lies in its ability to foster systemic change. By raising awareness and challenging existing norms, mental health advocates drive the development of innovative solutions such as enhancing Healthcare Provider Cultural Competency Training to better serve diverse communities or implementing Inner Strength Development programs that empower individuals to manage their mental health proactively. These efforts contribute to a more comprehensive and effective policy landscape, ultimately improving access to quality care and promoting mental wellness for all.
Castle Rock Chronic Pain Therapy: A Case Study in Policy Analysis and Advocacy Success

The Castle Rock Chronic Pain Therapy (CRCPT) program serves as a compelling case study in mental health policy analysis and advocacy success. This initiative, focused on providing specialized treatment for individuals suffering from chronic pain, exemplifies effective collaboration between healthcare providers, policymakers, and advocates. By integrating evidence-based practices and tailoring interventions to meet the unique needs of patients, CRCPT has significantly improved outcomes related to emotional healing processes and inner strength development.
The program’s success can be attributed to a multi-faceted approach that includes comprehensive risk management planning for mental health professionals, ensuring safety and sustainability in delivering care. Through robust policy analysis, advocates identified gaps in existing services and successfully lobbied for expanded coverage and increased access to specialized treatments. As a result, CRCPT has not only enhanced the lives of those dealing with chronic pain but also set a precedent for improving mental health service delivery on a larger scale, showcasing the power of advocacy in shaping policies that support emotional well-being.
Mental health policy analysis and advocacy play a pivotal role in ensuring equitable access to care. By understanding the impact of policies on mental health services, we can empower advocates to shape effective strategies. The case study of Castle Rock Chronic Pain Therapy demonstrates that collaborative efforts between professionals, policymakers, and community members can lead to successful outcomes, improving lives affected by mental health challenges. This approach encourages a holistic examination of existing policies, fostering systemic change for better mental well-being.